The world of medical billing and coding can be complex, with a myriad of rules, regulations, and codes to grasp. Nevertheless, navigating this system effectively is vital for healthcare providers to ensure accurate reimbursement for services rendered. This comprehensive guide provides valuable insights and strategies to enhance your medical billing and coding processes. From understanding the basic concepts to navigating specific coding scenarios, this guide serves as a trustworthy resource for both entrants and experienced professionals in the healthcare industry.
- We shall venture on this informative journey together.
Streamlining Provider Credentialing for Healthcare Success Bolstering
In today's rapidly evolving healthcare landscape, provider credentialing plays a crucial role in ensuring patient safety and operational efficiency. Streamlining this process can yield substantial benefits for both healthcare organizations and providers. A well-structured credentialing system reduces administrative burden, minimizes wait times, and fosters transparency. By embracing technology solutions and implementing best practices, healthcare institutions can optimize their credentialing workflows, enabling them to focus on delivering exceptional patient care.
- Leveraging automation tools can significantly reduce manual effort and improve accuracy in the credentialing process.
- Centralized credentialing databases allow for efficient tracking and management of provider information.
- Real-time communication and collaboration between stakeholders streamline workflows and accelerate approvals.
Furthermore, a robust credentialing system bolsters patient confidence by ensuring that providers meet established qualifications and adhere to regulatory requirements. By prioritizing provider credentialing, healthcare organizations can promote a culture of excellence and contribute to the overall success of their operations.
Interpreting Medical Terminology: Essential Knowledge for Billing and Coding
Accurate billing and coding in the healthcare industry hinge on a solid understanding of medical terminology. Caregivers utilize a specialized language to document patient encounters, procedures, and diagnoses. This complex lexicon can be complex for those unfamiliar with its intricacies.
Therefore, mastering medical terminology is essential for billing and coding specialists. It enables them to correctly translate clinical documentation into standardized codes used by insurance companies and government agencies. A comprehensive grasp of medical terms allows professionals to ensure accurate claims submissions, enhance reimbursement rates, and mitigate costly billing errors.
A strong foundation in medical terminology empowers billing and coding specialists to efficiently navigate the complexities of healthcare finance.
Submitting Medical Claims Masterfully
Effectively managing medical claims is a vital component of any healthcare provider's workflow. A well-structured and accurate claim secures timely payment from insurance providers. To master this art, it is vital to comprehend the intricacies of medical coding, billing procedures, and claim processing requirements.
- Familiarize with various insurance plan structures.
- Utilize automated billing software to enhance the claim workflow.
- copyright meticulous patient records to facilitate accurate coding and claim preparation.
Proactive follow-up on claim resolution is key to addressing any issues promptly. By adhering industry best practices and staying abreast about evolving regulations, healthcare providers can achieve efficient and consistent medical claim submission.
Enhancing Revenue Cycle Management Through Accurate Billing and Coding
Revenue cycle management (RCM) is a crucial aspect of healthcare finance. Accurate billing and coding are the foundation of an efficient RCM system, ensuring timely and appropriate payment from insurance providers and patients.
Establishing robust processes for billing and coding minimizes claim denials, streamlines the revenue cycle, and improves overall financial health.
By investing in accurate billing and coding, healthcare providers can maximize their revenue potential, bolster their financial outlook, and ultimately provide better patient care.
Influence of Provider Credentialing on Patient Access to Care
Provider credentialing procedures play a crucial get more info role in patient access to care. By assessing the qualifications and skills of healthcare providers, credentialing ensures that patients receive high-standard medical services. A robust credentialing process lowers the risk of incompetent care, defending patients from potential harm.
Patients benefit from a efficient credentialing process, as it facilitates timely access to their preferred providers. When provider information is up-to-date, patients can readily locate qualified healthcare professionals who meet their needs. Conversely, a burdensome credentialing process can create delays and hindrances to patient access, ultimately affecting the overall health outcomes of individuals and communities.
 Jaleel White Then & Now!
Jaleel White Then & Now! Tia Carrere Then & Now!
Tia Carrere Then & Now! Josh Saviano Then & Now!
Josh Saviano Then & Now! Sydney Simpson Then & Now!
Sydney Simpson Then & Now!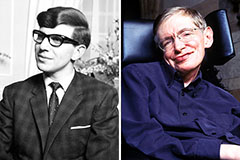 Stephen Hawking Then & Now!
Stephen Hawking Then & Now!